After confirming that my baby had died at 10 weeks back in 2013, I was left trying to deal with the loss both physically and emotionally. In an aim to help other women handle their tragedy, I’ve chosen to share my story from start to finish in a series of short articles, so that other women who face what our family did are more prepared. You’ll find my story enhanced with research as well as information gleaned from talking to other women who have had miscarriages and health care professionals I met through the process to help answer questions you may find yourself asking.
Article two addresses handling the grieving process. Our family, unfortunately, suffered two miscarriages at almost the same time. My sister-in-law also had a loss at 10 weeks, one month before my own. She and I handle grief in very different ways offering a perspective from two different ends of the emotional spectrum. I tend to be quite logical. If you can “make sense” of things for me, I can cope, while my sister-in-law tends to be more emotional and less concerned with the details.
What might help you deal with your miscarriage if you are a logical thinker:
For me, research is what helped. I wanted to know why my baby died, why after three healthy pregnancies, I lost the fourth with no warning whatsoever. I never found a factual answer, it is quite difficult to determine why a miscarriage happens, but the most common reason for miscarriage is chromosomal abnormality.
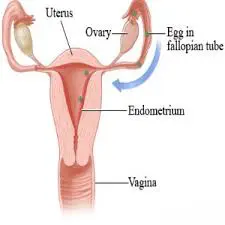
Chromosomes are kind of like the genetic blueprint your baby’s body follows while developing. Sometimes that blueprint may become damaged or be missing portions. This could be from damage to the sperm or egg, poor egg or sperm quality, or just a fluke; it just happens sometimes. This is most often the cause of missed miscarriage, as the baby begins to develop properly, but is unable to finish. As there is no trauma or placental issue, there is often no bleeding and the body goes right on thinking it’s pregnant for weeks. My baby’s passing was estimated to have occurred at 8 weeks, however, I didn’t fully miscarry naturally until 11 weeks with no bleeding until just past 10.
Some outside factors are also believed to increase the risk of miscarriage in general, including hormonal imbalance (particularly low progesterone), poor maternal health, smoking, drug use, and maternal age.
When I realized that had my baby lived, he or she may not have been healthy or may have had lifelong disabilities due to chromosomal abnormality, I felt better about my loss. I asked myself the question, “If I could have chosen, between a full-term baby that wasn’t healthy and a first trimester loss, which would I choose?” The answer was the loss. It still hurt, I still wished my baby would have been OK, healthy and happy, but knowing that the miscarriage was a mercy made it hurt a little less.
What might help you deal with your miscarriage if you are more emotionally driven:
For my sister, it helped to stay surrounded by the people she loved. She didn’t just keep us around to distract her, she talked about it. She posted on Facebook about it. She wrote about it. She did everything she could to let that emotion out. Think about how you’ve handled sadness at other times in your life; maybe you journaled, listened to music, created art, went out with your friends. While this loss is different and may hurt more than others you’ve survived, those same coping mechanisms are a good place to start if you’re looking for peace.
Above all, know that no matter how you handle grief, this was not your fault. You could not have stopped it, no matter how all-powerful moms seem to be. Things happen in life that are well beyond our control. What is in our control is how we handle them. This is not to say that you can turn off the hurt, but that like all wounds this one will heal, even if it leaves a nasty scar.
You can read the next article in this series which covers what a miscarriage is like here.