I remember the first time I experienced spotting during pregnancy. My heart dropped, and my mind automatically jumped to the conclusion I was miscarrying, but vaginal bleeding while pregnant is actually quite common. In fact, around 25 percent of women, or 1 in 4, experience it during the first 12 weeks of pregnancy.
Note: If you are not sure if you are pregnant and curious if what you are seeing is your period, implantation bleeding, or pregnancy spotting, you may find this page on what looks like a period while pregnant more helpful. This post is more aimed at spotting after a confirmed pregnancy in the first trimester. Bleeding during pregnancy in later trimesters is also covered here.
The probable causes of bleeding in pregnancy vary by what trimester it occurs in. This article covers three major time periods as well as the prevalence of pregnancy bleeding and risk factors. You can click any of the anchors below to jump to the section for your applicable stage of pregnancy or desired topic.
-In the first trimester (month 1 – 3)
-In the second and third trimester
-How common is pregnancy bleeding? What are the risk factors?
-Citation section
-Comments
Bleeding during pregnancy in the first trimester (First month to about month 3):
Cervical changes
Blood flow to the cervix (the opening between the vaginal canal and uterus) increases during pregnancy. This can make it more prone to minor damage. Things such as sex, dilation or position checks, PAP smears, and even excessive physical activity, which may have triggered small contractions, can cause spotting during pregnancy.
You should always mention any bleeding to your care provider, though short-term spotting is not often a cause for concern, especially if it was just once and after an activity that may have affected your cervix.
Progesterone dip
Around week 6 the placenta begins to take over production of progesterone. Sometimes during this time, there is a slight and temporary progesterone dip that can cause light bleeding in pregnancy. This is the most common time for spotting during pregnancy to occur.
Infection
Infections that may cause inflammation to the cervix or vaginal canal can also cause spotting during pregnancy. These may include common infections, such as yeast infections and bacterial vaginosis, as well as sexually transmitted diseases such as herpes, gonorrhea, and chlamydia. Spotting accompanied by foul-smelling discharge, itching, skin rashes, or warts may be a good tip-off this is what you’re dealing with, though not all infections present with symptoms.
Subchronic hematoma
A subchronic hematoma is a pocket of blood or blood clot within the uterine wall. This cause of spotting might sound a bit scary, but in most cases, subchronic hematomas are minor and resolve on their own. Bleeding from a uterine hematoma may be as light as spotting or heavy with clots depending on severity. Ultrasound is usually used to confirm that severity.
Hematomas are another type of pregnancy bleeding sometimes mistaken for a period because they can cause heavier and repeated bleeds. These bleeds would still not be rhythmic, occurring around the same time each month.
Ectopic pregnancy
Sadly, there are a few causes of spotting during pregnancy that are bad news. Ectopic pregnancy, where the baby has implanted somewhere outside of the uterus, such as the fallopian tube, is one of those causes. Ectopic pregnancy can cause long-term fertility issues and even be life-threatening, so the earlier it’s discovered, the better. Symptoms of ectopic pregnancy in addition to bleeding or spotting may include severe cramping, abdominal pain, lightheadedness, and a pregnancy test that is positive, then negative.
Molar Pregnancy
Keeping up with those bad news causes of spotting during pregnancy, molar pregnancy occurs when tissue (a tumor) begins to grow within the uterine wall causing a positive pregnancy test.
Molar pregnancies are rare and caused by chromosomal abnormalities within the fertilized egg. In addition to spotting, symptoms may include:
- Severe nausea or vomiting
- High blood pressure
- Measuring large (rapid uterine growth)
- Passing of cysts
- Pelvic pain or pressure
- Very high hCG levels
Miscarriage
Finally, spotting during pregnancy can indeed be caused by miscarriage, whether missed or impending. Keep in mind that in almost all cases, nothing was done to cause or can be done to prevent early miscarriage. The most common cause is chromosomal abnormality.
Bleeding during pregnancy in the second or third trimester
While bleeding during pregnancy during the first month of pregnancy, and throughout the first trimester even, is quite common and usually not cause for concern, most of the cases later in pregnancy are far rarer, but also often less benign, unfortunately.
Placenta abruption
Placental abruption occurs when the placenta partially or completely separates from the uterine wall before birth. This can deprive the baby of nutrients and oxygen. Minor abruptions can be managed with rest.
Uterine rupture
Uterine rupture is most common in women who have previously had a c-section and is rare even in that case. Uterine rupture happens most frequently during active labor and is life-threatening to both mother and child. Given this, it requires an emergency c-section.
Placenta Previa
Placenta previa occurs when the placenta partially or completely covers the cervix. Depending on the severity of placenta previa, treatment may range from bed rest at home without physical exertion or sex to emergency c-section.
Incompetent cervix:
An incompetent cervix, sometimes called a weak cervix, may attempt to open or open before the end of the pregnancy. This condition is present throughout pregnancy but isn’t typically symptomatic (causing bleeding during pregnancy) until the baby becomes large enough to begin placing weight on the cervix. Incompetent cervix is one of the most common causes of second-trimester losses. You may notice increased pressure as if your baby has dropped into your pelvis, a change in discharge prior to spotting or bleeding, back pain, or contractions. An incompetent cervix can be stitched to prevent preterm labor if caught early enough.
Miscarriage or Premature labor
Before 20 weeks, an attempted loss or loss is still referred to as a threatened miscarriage or miscarriage. After 20 weeks, it’s referred to as premature labor. All the above-mentioned causes of bleeding during pregnancy can also be a cause of miscarriage or preterm labor. Certain infections, abdominal trauma, and chromosomal abnormalities can also be to blame, but in other cases, no cause is known. Take heart, however, in knowing the current rate of miscarriage after a heartbeat is seen at 8 weeks is a mere 1 percent.
As mentioned earlier on this page, bleeding during pregnancy, any bleeding, no matter how slight, should be reported to your care provider. Light bleeding during pregnancy is very likely no cause for concern. Heavy bleeding can be more serious, but either way, better safe than sorry.
How common is bleeding during pregnancy?
Surprisingly, I wouldn’t say there are a wealth of studies on this subject. From 1983 to 2023, 18 studies could be found (a full list of studies used in this piece, including summaries and links, can be found at the end of this page).
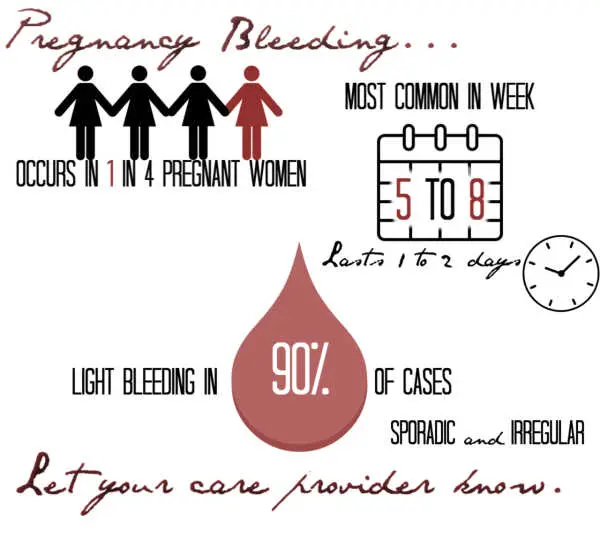
The observed rate of bleeding during pregnancy varied from 7 to 27 percent. As a result, 1 in 4 pregnant women is considered an accurate estimate by most sources for the prevalence of early pregnancy bleeding.
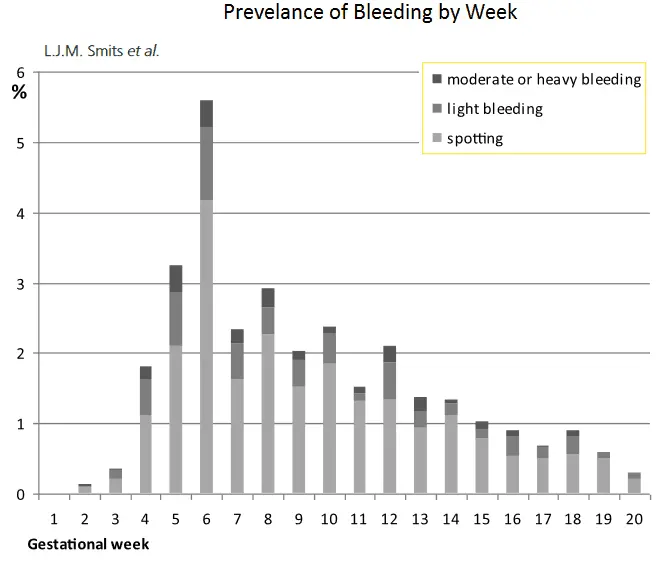
What type of bleeding is most common in pregnancy, and when it is most likely to occur?
Bleeding described as spotting or light accounts for roughly 90 percent of all pregnancy bleeding. Bleeding is most common in the first trimester, occurs only once, lasts one to two days, and is most frequently seen between weeks 5 and 8. This is suggested to be because around that time, the placenta takes over progesterone production, and a slight, temporary progesterone dip may result. It’s likely this common flow, duration, and timing is why so many women suspect they are still having or have had a light period.
Bleeding in pregnancy is sporadic, without a timely occurrence like a period, though episodes in the first trimester are also frequently seen around the time the next period after conception would have occurred.
What are the likely outcomes of pregnancy bleeding?
Unfortunately, in studies that examined the outcome of pregnancy bleeding, a similar pregnancy loss rate of around 50 percent was found. The rate of miscarriage in all pregnant women is estimated at between 10 and 25 percent, so it’s important to note that no studies found bleeding in pregnancy to cause miscarriage. Rather, it’s the other way around. Miscarriage is one possible cause of bleeding in pregnancy. Rates of loss were higher in those who experienced heavy bleeding and/or bleeding that exceeded 4 days.
In second-trimester bleeding, the chances of preterm labor, C-section, and low birth weight also increase.
What are the risk factors for bleeding during pregnancy?
Rates of bleeding in pregnancy are higher:
-In those older than 35
-When carrying multiples
-If you have had previous miscarriages
-When you have hormonal conditions or symptoms of hormonal imbalance, such as PCOS, fibroids, very long/short cycles, etc.
-If you have uterine abnormalities
-In those with diabetes
-With vaginal infections.
Studies on Bleeding During Pregnancy
Below is a list of studies done on bleeding during pregnancy with quick summaries of the rate of bleeding that was found and any other noteworthy points, such as when the bleeding occurred, whether it was light or heavy, how long it lasted, risk factors, etc.
Note: A University library login was used to read many of these studies. Some may not offer full access for free without a login. I only included studies here I was able to read. If you find others and would like them included, please contact me. The percentage shown in bold is the rate of pregnancy bleeding.
1983: Study of 16,305 women found a rate of bleeding of 14.6 percent. 91 percent experienced spotting only, and 8 percent heavy bleeding.
Berkowitz GS, Harlap S, Beck GJ, Freeman DH, Baras M. Early gestational bleeding and pregnancy outcome: a multivariable analysis. Int J Epidemiol. 1983;12:165–73
1984: Retroactive study of 7,486 women. 7 percent.
Batzofin JH, Fielding WL, Friedman EA. Effect of vaginal bleeding in early pregnancy on outcome. Obstet Gynecol. 1984;63:515–8.
1991: Study of 14,458 women. 17.6 percent. 55 percent of bleeding occurred in the first trimester. 6.82 percent light bleeding only.
Williams MA, Mittendorf R, Lieberman E, Monson RR. Adverse infant outcomes associated with first-trimester vaginal bleeding. Obstet Gynecol. 1991;78:14–8.
1992: Study of 8,718 women. 9.3 percent. 6.89 percent in the first trimester.
Sipila P, Hartikainen-Sorri AL, Oja H, Von Wendt L. Perinatal outcome of pregnancies complicated by vaginal bleeding. Br J Obstet Gynaecol. 1992;99:959–63.
1994: Meta-analysis of 28 studies from 1950-1992. 12.9 percent.
Ananth CV, Savitz DA. Vaginal bleeding and adverse reproductive outcomes: a meta-analysis. Paediatr Perinat Epidemiol. 1994;8:62–78.
1995: Study of 5,868 women. 19 percent. Bleeding was most common at 8 weeks, lasted no more than 2 days, and was a single occurrence.
Axelsen SM, Henriksen TB, Hedegaard M, Secher NJ. Characteristics of vaginal bleeding during pregnancy. Eur J Obstet Gynecol Reprod Biol. 1995;63:131–4.
1997: Study of 550 women. 21 percent.
Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997;315:32–4.
1999: Study of 1,100 women. 11 percent. Vaginal infection found to be a risk factor.
French JI, McGregor JA, Draper D, Parker R, McFee J. Gestational bleeding, bacterial vaginosis, and common reproductive tract infections: risk for preterm birth and benefit of treatment. Obstet Gynecol. 1999;93:715–24.
2001: Study of 7,658 women. 14.4 percent. Preterm birth was more common in those with early pregnancy bleeding.
Yang J, Savitz D. The effect of vaginal bleeding during pregnancy on preterm and small-for-gestational-age births: US National Maternal and Infant Health Survey, 1988. Paediatr Perinat Epidemiol. 2001;15:34–9
2003: Study of 221 women before pregnancy. 68.3 percent (151) became pregnant. 9 percent had bleeding before 8 weeks. Data was not continued beyond 8 weeks.
Harville EW, Wilcox AJ, Baird DD, Weinberg CR. Vaginal bleeding in very early pregnancy. Hum Reprod. 2003;18:1944–7.
2004: Screening of 16,506 women. 14.38 percent. Light bleeding accounted for 12.86 percent, heavy bleeding 1.52 percent.
Weiss JL, Malone FD, Vidaver J, et al. Threatened abortion: A risk factor for poor pregnancy outcome, a population-based screening study. Am J Obstet Gynecol. 2004;190:745–50.
2005: Study of 2,806 women. 24.48 percent. 77.4 percent occurred in the first trimester. 69.9 percent had only one episode of bleeding. 79.3 percent light bleeding only. Risk factors including older maternal age and previous miscarriage.
Yang J, Savitz DA, Dole N, et al. Predictors of vaginal bleeding during the first two trimesters of pregnancy. Paediatr Perinat Epidemiol. 2005;19:276–83.
2007: Study of 2,678 women. 26 percent. 83.6 percent of which occurred in the first trimester.
Hossain R, Harris T, Lohsoonthorn V, Williams MA. Risk of preterm delivery in relation to vaginal bleeding in early pregnancy. Eur J Obstet Gynecol Reprod Biol. 2007;135:158–63.
2009: Study of 4,510 women. 27 percent. 42.9 percent of those with bleeding miscarried. Only 8 percent saw heavy bleeding. Episodes of heavy bleeding correlated with a three times higher chance of miscarriage, while episodes of light spotting showed no difference in comparison to those who experienced no bleeding.
Hasan R, Baird DD, Herring AH, Olshan AF, Jonsson Funk ML, Hartmann KE. Association between first-trimester vaginal bleeding and miscarriage. Obstet Gynecol. 2009;114:860–7
2010: Study of 4,539 women. 12 percent ended in miscarriage with about 2 in 3 experiencing bleeding prior to their loss. These losses were excluded from the rate of bleeding in pregnancy given, which was 25 percent. 75.6 percent of bleeding was light. 71 percent of bleeding occurred only once. Risk factors included prior miscarriage, advanced maternal age, fibroids, blood sugar issues, and signs of hormonal imbalance. The rate of loss was higher in those with heavy bleeding.
Hasan R, Baird DD, Herring AH, Olshan AF, Jonsson Funk ML, Hartmann KE. Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Annals of epidemiology. 2010;20(7):524-531.
2010: Study of 2,054 women. 23.9 percent. Most episodes were light bleeding in the first 20 weeks.
Skorokhod, Veronika. Vaginal Bleeding during the First 20 Weeks of Pregnancy and the Risk of Preterm Delivery, Michigan State University, Ann Arbor, 2010, ProQuest Dissertations & Theses Global.
2011: Study of 3,431 women. 23 percent. 72 percent of bleeding occurred in the first trimester with week 6 being most common. 73 percent occurred only once. 90 percent of bleeding was light.
Smits LJM, North RA, Kenny LC, Myers J, Dekker GA, Mccowan LME. Patterns of vaginal bleeding during the first 20 weeks of pregnancy and risk of pre-eclampsia in nulliparous women: results from the SCOPE study. Acta Obstet Gynecol Scand 2012.
2017: Study of 11,835 women. 8.5 percent. 84 percent of those later miscarried. Bleeding prior to 6 weeks was more likely to lead to loss. Bleeding was also most common prior to 6 weeks. 83.2 percent experienced only spotting, 16.8 percent heavy bleeding, and the miscarriage rate was higher in those with heavy bleeding.
Kamble PD, Bava A, Shukla M, Nandanvar YS. First trimester bleeding and pregnancy outcome. Int J Reprod Contracept Obstet Gynecol 2017;6:1 48-7.
Note:
I do my best to respond to comments within 48 hours. All comments are moderated. Please remember, I am not a doctor nor a replacement for medical care. I can’t tell you what’s causing your spotting over the internet. I do have a medical background (medical assisting) and am a mother of four who struggled with infertility as well as multiple miscarriages. However, I am not a doctor nor claim to be one.
You may also find helpful:
Period While Pregnant
Early Signs of Pregnancy Quiz
When Do Pregnancy Symptoms Start?
Period Blood Colors and Textures Explained